Post script for "Fat vs. Fat, and Insulin Resistance"
I can't get this out of my mind, so I'm putting it here...
So there are a couple of oddities about (Xiao, 2006) that I can’t get out of my mind, but that don’t really pertain to the substance of the analysis of that study. I had included them in the post, and then edited them out.
Fat vs. Fat, and Insulin Resistance
Introduction Peter looks at a study today in which various fats are tested to see how they do in inducing insulin resistance: “Protons (72) Humans: 8% LA [Linoleic acid] Vs 74% LA by Sustained Oral Ingestion” (Dobromylskyj, 2024b) He’s looking at this paper: “
But I keep thinking about them…
In the previous post I note that (Xiao, 2006) was examined by the authors of (Nowotny, 2013) who observed that their results were the exact opposite.
There was another study that found that (Xiao, 2006) was an outlier.
“Compared with SAF, PAL had a somewhat more pronounced inhibitory effect on insulin sensitivity during the clamp test, with reduction in insulin-stimulated NOXGD as well as glucose disposal during the basal period of fasting insulinaemia, as seen in most [5, 11] but not all human studies [12].” (Sarabhai, 2022)
[12] is (Xiao, 2006). The ‘basal’ period they are referring to is that period after the initiation of the experiment—after the ‘pre-basal’ phase, confusingly—but prior to the clamp.
Aside:
This is another aggravating study. At first glance, it appears to replicate (Xiao, 2006) because it is comparing palm oil (PAL), the SFA in Xiao, with safflower oil (SAF) the PUFA in Xiao. What’s not mentioned explicitly anywhere in the text is that they’re using a low-linoleic, high-oleic version of safflower oil:
“…SAF ~1.18 g/kg BW (8% saturated FA, 65% monounsaturated FA, 23% polyunsaturated FA; Mazola, Elmshorn, Germany)…” (Sarabhai, 2022)
So what they’re really doing is comparing the SFA to the MUFA arm of (Xiao, 2006). Are they aware of this difference? Are they doing this to obfuscate something? It’s impossible to know.
However, they do measure the increase in LA from these two oils, and it’s almost identical, as you would expect.
“Plasma linoleic acid rose by ~82% after SAF and by ~78% after PAL, compared with VCL (p = 0.001 and p = 0.036, respectively; Fig.2f).” Control was water, again.
The blood glucose during the clamp is also almost identical, as it should be. They don’t disclose the infusion rates.
End Aside.
Funding for the first two studies (Carpentier, 1999; 2000) was primarily from the “Eli Lilly Banting and Best Diabetes Research Program at the University of Toronto”. Eli Lilly is, of course, a drug company that makes insulin. (Xiao, 2006) was funded by the Canadian Diabetes Association. Does that make a difference? The Canadian Diabetes Association has changed its name to Diabetes Canada, but it still advises that one:
“Select unsaturated oils and nuts as the preferred dietary fats.”
“The DRIs also recommended that the percentage of total daily energy from CHO should be ≥45% to prevent high intake of saturated fatty acids as it has been associated with reduced risk of chronic disease for adults.”
And does the usual fear-mongering about low carbohydrate diets. (Diabetes Canada Clinical Practice Guidelines Expert Committee, 2018)
So yes, a paper that showed the superiority of a high-PUFA diet in diabetes would have been popular! That’s just speculation, however, but it is odd.
Here’s what’s really interesting, and I should have checked this prior to finishing yesterday’s post.
Xiao and Lewis produce a subsequent study looking at insulin resistance and dietary fats in 2009, three years later. (This was also funded by the Canadian Diabetes Association.) Obviously they don’t use a high-PUFA diet, since they’ve shown that to induce insulin sensitivity, right?
They would use palm oil.
Nope, they’re back to infusing soybean oil in Intralipid. And note: unlike in (Carpentier, 1999), they’re using “overweight and obese nondiabetic men”, just like in (Xiao, 2006), so my speculation that the insulin ‘sensitivity’ as evidenced by increased glucose infusion may have been an artifact of the subjects’ health is defeated.
A high-PUFA fat seems to again induce insulin resistance. In (Xiao, 2009) they also cite their previous paper, (Xiao, 2006) as reference 53:
“Higher insulin levels in the IH and SS treatment groups combined with similar insulin secretion rates suggests decreased insulin clearance. This was confirmed by the significantly lower calculated insulin clearance rates in IH, IH + SS, and SS studies compared with SAL (P < 0.05; Fig. 2D). Decreased insulin clearance was shown in our previous studies after 24-h oral fat ingestion (53) or 48-h IH infusion (10, 11).” (Xiao, 2009)
They explain the significant of insulin clearance:
“The reduction in insulin clearance contributes to peripheral hyperinsulinemia, which can erroneously be interpreted as an increase in insulin secretion unless accompanied by an increase in plasma C-peptide concentrations or calculated insulin secretion rate, as we have done in the present study….” (Xiao, 2009)
Indeed, in (Xiao, 2006) PUFA had the lowest C-peptide value.
This directly pertains to the glucose infusion rate, as we discussed in the previous post:
“In addition, measurements of glucose disposal must be assessed in relation to circulating insulin concentration. If this calculation is not performed, as we have done in the present study, the increased glucose disposal associated with higher circulating insulin concentrations may be misinterpreted as improved insulin sensitivity.” (Xiao, 2009)
They described this impaired insulin clearance in the 2006 paper:
“Insulin clearance calculated from the last 30 min of the 20-mmol/l hyperglycaemic clamp was significantly impaired with ingestion of all three fats. The impairment was greater with PUFA than with SFA or MUFA (†p<0.001 vs control, ‡p<0.001 vs SFA and MUFA)” (Xiao, 2006)
See the above graph, and Fig. 2c:
In light of the following paragraph from (Xiao, 2009):
“In our study, the glucose infusion rates might have been even lower had the insulin levels not increased due to the impaired insulin clearance. Insulin clearance is mediated by similar and partly overlapping pathways affecting insulin sensitivity, and indeed salicylate also decreased insulin action.”
What is the significance of insulin clearance in the context of type 2 diabetes?
“Thus, data from human volunteers confirms a wide variance in first-pass hepatic insulin extraction and supports the idea that lower insulin clearance is characteristic of individuals at increased risk for type 2 diabetes.” (Bergman, 2022)
Interesting, given that we see here that increased Ω-6 fats causes insulin resistance, worsened insulin clearance, and also obesity.
What Is The Most Fattening Food?
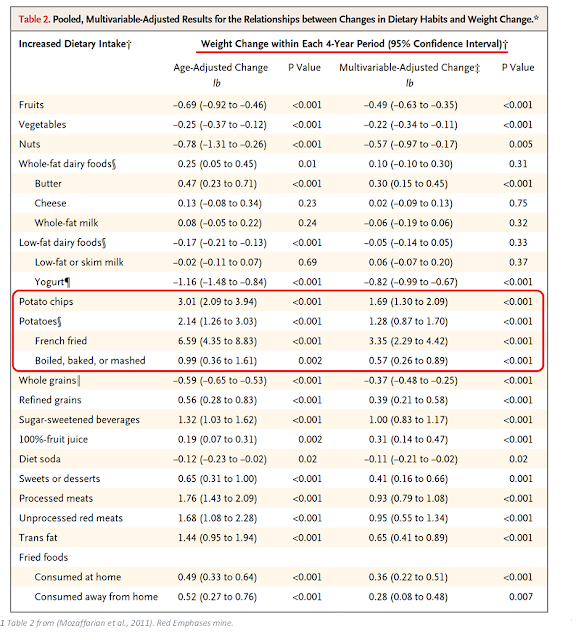
I came across this paper recently: "Changes in Diet and Lifestyle and Long Term Weight Gain in Women and Men” (Mozaffarian et al., 2011) From the illustrious New England Journal of Medicine.Thanks for reading Tucker Goodrich: yelling Stop! Subscribe for free to receive new posts and support my work.
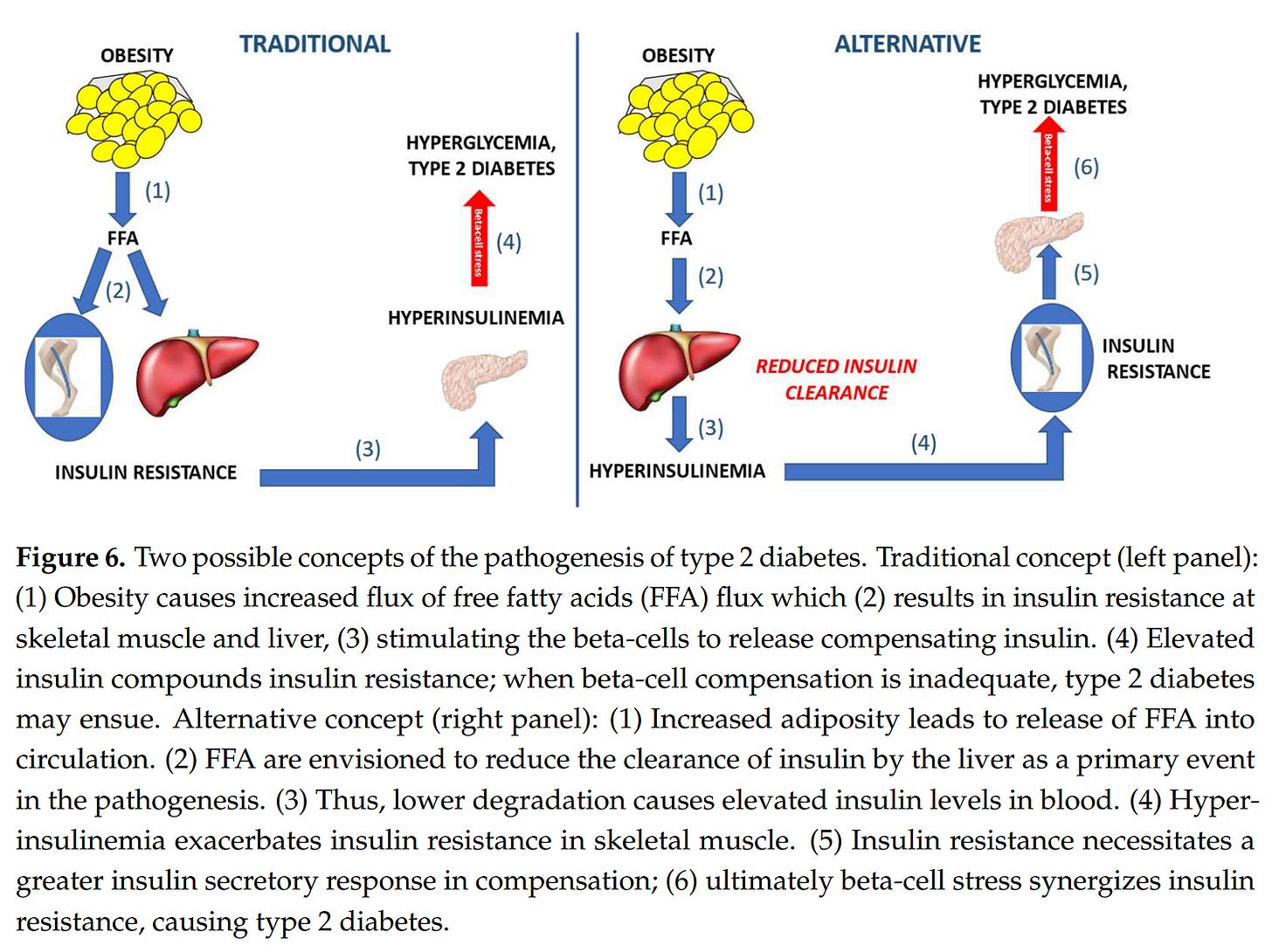
It suggests they are parallel processes, as we see in lean type 2 diabetes, and not serial, as shown here.
So the takeaway here is clear, and while Peter and I will continue to discuss the details of what is happening, we agree: “But the convergence is to the marked reduction of linoleic acid ingestion.”
References
References not found here are in the previous post.
Bergman, R. N., Kabir, M., & Ader, M. (2022). The Physiology of Insulin Clearance. International Journal of Molecular Sciences, 23(3), Article 3. https://doi.org/10.3390/ijms23031826
Diabetes Canada Clinical Practice Guidelines Expert Committee. (2018). Chapter 11: Nutrition Therapy. In Diabetes Canada 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Diabetes Canada. https://guidelines.diabetes.ca/cpg/chapter11
Xiao, C., Giacca, A., & Lewis, G. F. (2009). The Effect of High-Dose Sodium Salicylate on Chronically Elevated Plasma Nonesterified Fatty Acid-Induced Insulin Resistance and Β-Cell Dysfunction in Overweight and Obese Nondiabetic Men. American Journal of Physiology. Endocrinology and Metabolism, 297(5), E1205-1211. https://doi.org/10.1152/ajpendo.00313.2009









Insulin also controls LPL and HSL thus a regulatory input of the assembly and disassembly of FFA thus controlling FFA. Is this regulation more important than regulating glucose? Which has priority?
Insulin sensitivity is defined via glucose - but regulating FFA might dominate the nested control loops.
T2D appears to be permanent damage - I'm still not sure which tissue is damaged - My hunch is the liver - but could be pancreas, muscle, adipose. Transplant data in humans doesn't clear this up.
Sometimes I think the studies are designed to NOT provide definitive answers. They used to do chemically defined synthetic diets where you could truly have a single variable.
Don't underestimate ignorance of nutrition/fat details in scientists. Like Speakman conflating things about fatty acids in your recent podcast.
Even Lamming, one of the BCAA mouse scientists I admire most, was like "Wait lard has linoleic acid?" when I commented that ALL his mice were PUFA'd, and that BCAA's effects might be in the context of LA only. And like your one guest mentioned once, scientists usually have no clue what's in their control chow either.