Fat vs. Fat, and Insulin Resistance
tl;dr: Fats induce insulin resistance in different ways at different times...
Introduction
Peter looks at a study today in which various fats are tested to see how they do in inducing insulin resistance:
“Protons (72) Humans: 8% LA [Linoleic acid] Vs 74% LA by Sustained Oral Ingestion” (Dobromylskyj, 2024b)
He’s looking at this paper: “Differential Effects of Monounsaturated, Polyunsaturated and Saturated Fat Ingestion on Glucose-Stimulated Insulin Secretion, Sensitivity and Clearance in Overweight and Obese, Non-Diabetic Humans” (Xiao, 2006).
After presenting this graph, Peter summarizes:
“I don't think I have to make any qualifications here. SFA oral ingestion for 24h causes a very similar degree of insulin resistance to oral ingestion of a minimal calorie supplying control chocolate drink. Tallow rather than palm oil would have accentuated the effect.
“Ingesting 70% of your calories as linoleic acid over a 24h period is insulin sensitising compared to ingesting SFA, p less than 0.001. Or ingesting virtually nothing at all, p < 0.05.
“Linoleic acid is insulin sensitising.”
The chart is showing that a higher amount of glucose must be infused to maintain a constant level of glucose in the blood (a “hyperglycaemic clamp”) for MUFA (monounsaturated fat) and PUFA (polyunsaturated fat) vs CONTrol, and that a lower level of glucose is required for SFA (saturated fat), suggesting that disposal of glucose in impaired by SFA, and that this reduced disposal represents insulin resistance (which is the inverse of insulin sensitivity). Or as Peter put it in the previous post “The higher the [glucose] infusion rate, the more insulin sensitive the rat is.”, looking at rats rather than humans (Dobromylskyj, 2024a)
Papers like this are the reason why it is claimed that saturated fats induce insulin resistance, with the suggestion that our high consumption of SFA is to blame for our epidemic of insulin resistance and thus type 2 diabetes, typified by insulin resistance. Wolpert in 2013, citing (Xiao, 2006)—ref 28, states, “Studies in nondiabetic individuals indicate that saturated fats cause more profound insulin resistance than monounsaturated and polyunsaturated fats (28,29).”
Let’s dig in…
Let’s consider the methods. For starters, the participants were “overweight and obese”.
“We elected to study overweight and obese, non-diabetic humans because we have previously shown that they are more susceptible to the impairing effect of chronically elevated fatty acids on GSIS than lean, insulin-sensitive individuals [13].” (Xiao, 2006)
What were these people eating, and how?
“On each occasion, participants ingested a hot, chocolate-flavoured drink consisting of either one of three fat emulsions (oil tests) or of water (control) every hour for the first 12 h followed by every 2 h for the remainder of the study, continuing through the clamp studies that began at 08.00 h on day 2 (i.e. the emulsion was ingested for a total of 30 h).” (Xiao, 2006)
So they were sleep- and protein-deprived for the 30 hours of the test, and were put on a high-fat diet to which they were likely not adapted. Additionally, they were lipid-engorged for ~24 h prior to the initiation of the glucose test—they arrived at 7am, and the test started at 8am the following morning.
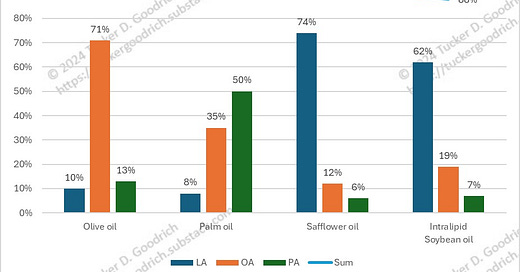
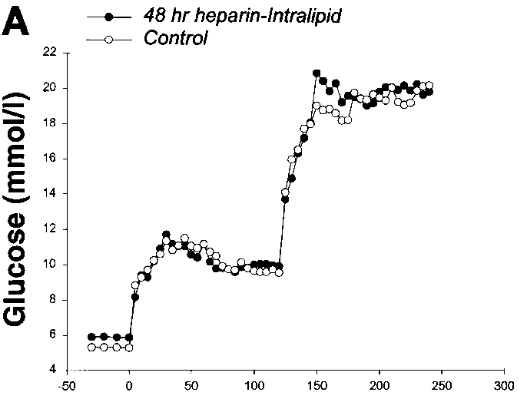
The three oils used in the study were olive oil (78% [MUFA], 8% [PUFA] and 14% [SFA]; 71% oleic acid, 13% palmitic acid and10% linoleic acid; referred to as MUFA), palm oil (50% [SFA], 40% [MUFA] and 10% [PUFA]; 48% palmitic acid, 35% oleic and 8% linoleic acid; SFA) and safflower oil (78% [PUFA], 13% [MUFA] and 9% [SFA]; 74% linoleic acid, 12% oleic acid and 6% palmitic acid; PUFA). We acknowledge that palm oil contains not only SFA but also a fair amount of MUFA. In the control test, oil was replaced with water. (Xiao, 2006)
They don’t describe how they know what the fats were in these three oils, as olive oil, for instance, varies from 3% to 23% linoleic acid (Hernández, 2021), and they don’t specify that they tested the oils, so we must assume that they used a database (USDA) to acquire that data, as this is the standard method. The FA levels are therefore approximate, but are specific enough to be useful as described, PUFA vs. MUFA vs. SFA. (We should note that there appears to be some interaction between the different fats, as the PUFA levels in olive oil and palm oil are similar, but the results are not.)
These authors (senior and corresponding author here was Gary Lewis) performed a previous study, (Carpentier, 1999) which they mention as the source for the information on how the hyperglycaemic clamp was performed.
Those participants were lean, “Sixteen healthy male research volunteers participated in the study.”
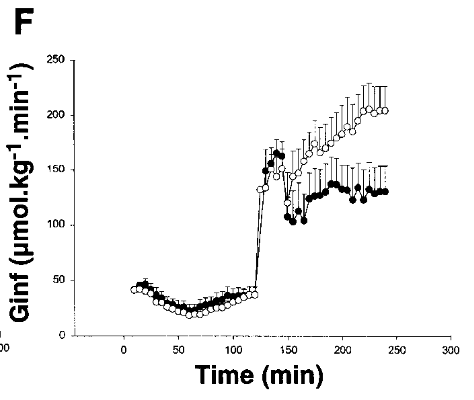
They either got a control diet or a lipid infusion of soybean oil, Intralipid (Sigma-Aldrich, Inc, 2020), in what’s known as a ‘cross-over’ design, all the participants got both interventions, with a long wash-out period in between.
“Each subject was studied on at least two occasions, 6–8 wk apart (some subjects participated in a third study outlined in Acute heparin-Intralipid studies). Eight of the sixteen subjects underwent a graded glucose infusion with and without a prior 48-h infusion of heparin and Intralipid, and the other eight subjects underwent a two-step hyperglycemic clamp, with and without a prior 48-h infusion of heparin and Intralipid.” (Carpentier, 1999)
I’ll ignore the details of the control diet (they’re not really provided, but they claim the same diet was used to prepare the Intralipid group). It was a high-carb diet.
Like the fats above, the composition of soybean oil can vary, so take this as representative, the important trait is that they tend to be high in LA. (All these fats have other components that are not listed for the fats in (Xiao, 2006), which is why they don’t sum to 100%.)
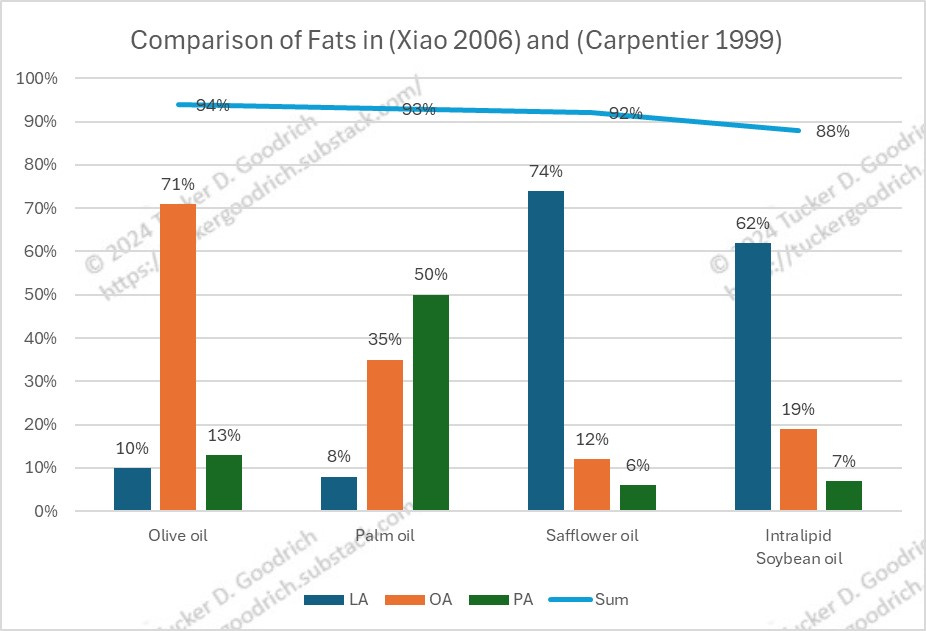
Carpentier in 1999 also showed the glucose infusion rates for Intralipid vs. control.
Comparison
I filled the PUFA column in the chart on the left to match the style on the right, where LA (in Intralipid) is colored black. As you can see, the glucose infusion rate for the control is lower on the left (my added green line) at around 42, vs. around 58 for the PUFA; and higher on the right, around 200 vs around 130 for the Intralipid. This suggests, as confirmed by the text in the relative papers, that soybean oil (right) is causing insulin resistance, and safflower oil (left) is causing the reverse effect, insulin sensitivity, despite their similar fat profiles.
Xiao says they’ve truncated their data to only that obtained, “during the last 30 min of the 20-mmol/l hyperglycaemic clamp.” Carpentier also performed this test (the reference used for Xiao, “At approximately 08.00 h a 2 h ,20 mmol/l hyperglycaemic clamp study was conducted as previously described [15]. Reference 15 is Carpentier, “We used two methods of determining GSIS: a programmed intravenous glucose infusion, which raises plasma glucose in a graded fashion to ~10 mmol/l, and a two-step hyperglycemic clamp to determine GSIS in response to plasma glucose concentrations as high as 20 mmol/l.”
It’s odd that the amount of glucose required to be infused during Carpentier was ~4x as high for the control as during Xiao, to reach the same amount of blood glucose.
The values during the last 30 minutes in the two papers are wildly different, and no explanation is offered as to why this might have been the case. During the earlier part of the two-step infusion, the values in the earlier, 10-mmol/l clamp, the earlier values for 10-mmol/l do seem to correspond with the latter values for 20-mmol/l, although that should not be the case.
The control used in Carpentier was a control diet, with no infusion at all. The control used in Xiao was the same drink as the intervention, with water instead of oil. It’s hard to fathom how the drink in Xiao could have such a remarkable insulin sensitizing effect, once the oil is removed.
Now the obvious difference between these two tests is that (Xiao, 2006) used an 24-hour oral delivery, and (Carpentier, 1999) used a 48-hour IV infusion. As Xiao explains:
“Previous studies, including our own, that have examined the effect of prolonged elevation of NEFAs on beta cell function and whole-body insulin sensitivity in humans have been performed by infusing a triglyceride emulsion, such as Intralipid, together with a continuous low-dose heparin infusion [13, 15, 20–23]. Because we specifically wished to compare the effect of SFA, MUFA and PUFA on insulin secretion, sensitivity and clearance in the present study and for the other reasons outlined in the Introduction, we turned to a method of oral fat ingestion recently described by Beysen et al. [11], in which the authors examined the stimulatory effects of an acute elevation of various fatty acids on insulin secretion.”
So is that it? IV infusion causes the reverse effect to oral ingestion?
Does it replicate?
Later authors have examined this. Describing (Xiao, 2006), the authors of (Nowotny, 2013) state:
“An hourly intake of oil enriched in polyunsaturated (78%), monosaturated (78%), or saturated FA (50%) over 12 h increased plasma FA starting at 8 h after the first dose and resulted in higher glucose infusion rates during clamps after ingestion of polyunsaturated, but not monosaturated or saturated, FA after 24 h (28).
“In contrast, the current study demonstrates a profound reduction of insulin sensitivity at 6–8 h after single ingestion of soybean oil rich in polyunsaturated FA (61%), which was used in order to match for the composition of the iv fat solution known to rapidly induce insulin resistance in humans [Intralipid] (6,7).”
They speculate:
“The seemingly contradictory findings probably result from different time intervals between fat ingestion and assessment of insulin sensitivity, differences in timing of fat application, its composition, and the absolute plasma FA concentration achieved (26,29).”
They go on to further explore the, “Mechanisms Underlying the Onset of Oral Lipid–Induced Skeletal Muscle Insulin Resistance in Humans”, and point the finger at linoleic-acid-containing di-aclyglycerides (DAG) stimulating the immune system.
Xiao authors note the shortcoming in their own methodology:
“We cannot with confidence exclude impairment of insulin sensitivity with the ingestion of PUFA or MUFA, however, because insulin sensitivity was not determined using a gold standard in vivo experimental technique, such as the euglycaemic hyperinsulinemic clamp.”
Xiao’s source for their testing methodology, (DeFronzo, 1979) describes this as a problem, as the test used is a method for measuring glucose metabolism, and not insulin sensitivity. While it often correlates well with the more accurate method, it’s not guaranteed.
Conclusion
The divergent results between two papers from the same group suggests that this may be a result specific to non-diabetic overweight individuals, although the lack of insulin sensitivity demonstrated by the high glucose levels produced by low glucose infusion rates are hard to reconcile with the participants being non-diabetic.
The divergent results between this paper and other papers, including from the same group, showing that fats with a similar lipid composition produce insulin resistance are hard to reconcile.
Especially hard to reconcile is the notion that saturated fat is the underlying cause of insulin resistance, and that linoleic acid is insulin sensitizing, as the ecological evidence indicates the reverse.
With respect to Peter, I will have to consider this result an outlier absent some convincing reconciliation between this result and the contradictory ones.
P.S.
Post script for "Fat vs. Fat, and Insulin Resistance"
So there are a couple of oddities about (Xiao, 2006) that I can’t get out of my mind, but that don’t really pertain to the substance of the analysis of that study. I had included them in the post, and then edited them out. But I keep thinking about them…
References
Carpentier, A., Mittelman, S. D., Lamarche, B., Bergman, R. N., Giacca, A., & Lewis, G. F. (1999). Acute enhancement of insulin secretion by FFA in humans is lost with prolonged FFA elevation. The American Journal of Physiology, 276(6), E1055-1066. https://doi.org/10.1152/ajpendo.1999.276.6.E1055
DeFronzo, R. A., Tobin, J. D., & Andres, R. (1979). Glucose clamp technique: A method for quantifying insulin secretion and resistance. The American Journal of Physiology, 237(3), E214-223. https://doi.org/10.1152/ajpendo.1979.237.3.E214
Dobromylskyj, P. (2024, May 30). Hyperlipid: Protons (71) Rats: 13% LA vs 61% (mostly) LA by infusion [Blog]. Hyperlipid. https://high-fat-nutrition.blogspot.com/2024/05/protons-71-rats-13-la-vs-61-mostly-la.html
Dobromylskyj, P. (2024, May 30). Protons (72) Humans: 8% LA vs 74% LA by sustained oral ingestion [Blog]. Hyperlipid. https://high-fat-nutrition.blogspot.com/2024/05/protons-72-humans-8-la-vs-74-la-by.html
Hernández, L., Sicardo, M., Belaj, A., & Martínez-Rivas, J. (2021). The Oleic/Linoleic Acid Ratio in Olive (Olea europaea L.) Fruit Mesocarp Is Mainly Controlled by OeFAD2-2 and OeFAD2-5 Genes Together With the Different Specificity of Extraplastidial Acyltransferase Enzymes. Frontiers in Plant Science, 12. https://doi.org/10.3389/fpls.2021.653997
Sarabhai, T., Koliaki, C., Mastrototaro, L., Kahl, S., Pesta, D., Apostolopoulou, M., Wolkersdorfer, M., Bönner, A. C., Bobrov, P., Markgraf, D. F., Herder, C., & Roden, M. (2022). Dietary Palmitate and Oleate Differently Modulate Insulin Sensitivity in Human Skeletal Muscle. Diabetologia, 65(2), 301–314. https://doi.org/10.1007/s00125-021-05596-z
Sigma-Aldrich, Inc. (2020, November 11). Intralipid: I141 [Advertisement]. Sigma-Aldrich, Inc. https://www.sigmaaldrich.com/catalog/product/sigma/i141
Wolpert, H. A., Atakov-Castillo, A., Smith, S. A., & Steil, G. M. (2013). Dietary fat acutely increases glucose concentrations and insulin requirements in patients with type 1 diabetes: Implications for carbohydrate-based bolus dose calculation and intensive diabetes management. Diabetes Care, 36(4), 810–816. https://doi.org/10.2337/dc12-0092
Xiao, C., Giacca, A., Carpentier, A., & Lewis, G. F. (2006). Differential Effects of Monounsaturated, Polyunsaturated and Saturated Fat Ingestion on Glucose-Stimulated Insulin Secretion, Sensitivity and Clearance in Overweight and Obese, Non-Diabetic Humans. Diabetologia, 49(6), 1371–1379. https://doi.org/10.1007/s00125-006-0211-x







It appears as if a lot of effort has gone into making what we know unknowable based on the way they design these studies? Lots of money spent - how is it that we don't have enough proper science to clearly answer these questions?
I would note that people with T2D probably have accumulated damage to their livers (and possibly pancreas). So there are two questions - Do PUFAs cause inappropriate insulin sensitivity in healthy people? and do PUFAs cause inappropriate insulin sensitivity in people with the damage that causes T2D. (Sadly, I think the damage is permanent). People with T2D end up with chronically elevated insulin levels.
So Tucker seems to be asking if the change in insulin sensitivity is immediate or generated over the course of long term exposure to PUFAs that damage tissues?
All these questions could be answered using synthetic diets ( as in Vivonex 100, Winitiz, Greenstien etc). Real experimental science varies only one variable at a time. Using diets that are not chemically defined does not help us much - we are left guessing if the results are due to one component while several are changed at once.
The other issue is that different tissues have different insulin sensitivity - but that is not the case. The tissues in the liver/adipose/muscles do not respond the same. And - the assumption that insulin is only involved with glucose is just wrong - but leads to the assumption that insulin sensitivity for glucose is the same as for triggering fat storage.
It turns out that BOTH high levels of LA and fructose can damage the liver - but what is particularly interesting is that the damages don't just add. This begs the question if the ongoing T2D pandemic might be caused by the combination of high PUFA + high fructose found in the average Western diet.
“On each occasion, participants ingested a hot, chocolate-flavoured drink consisting of either one of three fat emulsions (oil tests) or of water (control) every hour for the first 12 h followed by every 2 h for the remainder of the study, ..." I feel sick just thinking about that.
Surely the correct way to get a correct result is to have people eating normally with controlled diets and then do a standard insulin response test. Also, long term is what we want to know about not some short trial where there could be short term metabolic responses to a very unnatural eating pattern.