Can a Low-Carb American Diet Cause Omega-3 Deficiency?
tl;dr: It would be nice if our food supply was trustworthy.
Dr. Michael Eades has done a number of posts recently about seed oils:
I thought I would do one about him.
I’ve had the privilege to meet him in person, and share a meal with him and our wives, at the AHS 2021 seminar where we both gave talks.
He’s a very smart guy. He’s one of the most knowledgeable people I know in the nutrition space, and has been one of the leaders of the low-carb community for decades.
He’s also very successful, and, to infer from the lifestyle comments he makes on his blog/newsletter The Arrow, can likely afford to eat as well as he thinks is necessary for his and his wife’s health (her nickname is “MD”).
Ω-3 Deficiency
So I was pretty surprised to read this:
“I have had a couple of problems I’ve been battling. One is a terrible itch on my back and the cheeks of my rear end. I’ve written it off to the dry skin of old age. MD keeps telling me to put some kind of skin conditioner on my back and butt, but I just don’t want to oil myself up. So I don’t. I also have mild back pain, probably from golf and doing dead lifts with the bands. My back is ancient and has suffered a lot of abuse over my fairly active life.”
Itchy skin (dermatitis) is a classic sign of essential fatty acid (EFA) deficiency. Ralph Holman was one of the more productive researchers in this area. He invented the Ω terminology we use to describe these fats, and described the first reported case of Ω-3 deficiency in a human being (Holman, 1982).
He described a “severe dermatitis of deficiency” which appeared when rats were made deficient in essential fats.
“When such rats were supplemented with marine (fish) oils, remarkable cures of dermatitis took place although such oils do not show curative activity in the usual assay.” (Holman, 1971)
For many decades it was thought that only rodents were subject to EFA deficiency, but the development of total parenteral nutrition (TPN), which was initially a fat-free formulation, proved that humans are susceptible to EFA deficiency too. A totally fat-free diet (the ultimate ultra-processed diet) induces “skin lesions” or “dermatitis” in a month or three.
Dr. Eades will be happy to hear that therapeutic administration of corn oil to the skin was ineffective: you are better off eating your ‘skin lotion’ (not literally) than applying it topically (Holman, 1998).
“MD and I started the sardines once a day and the flaxseed oil salad dressing with every meal, and my itching vanished within a week. I kid you not. And my back pain is all but gone.”
Sardines, of course, contain the animal-based Ω-3 fats we actually need; flaxseed oil contains plant-based Ω-3 fats that we can convert to the animal-based ones. Somewhat. See the FADS research below.
So that, to me, seems to be a pretty clear case of a deficiency which is immediately cleared up by curing the deficiency. Dr. Eades seems to think the same.
“So, in the words of the famous Monkee’s song, ‘now I’m a believer. Not a trace of doubt it my mind.’ Just adding that bit of omega-3 to my diet has paid huge dividends…. I do know it got rid of my chronic itch and my back pain and did so quickly.”
And yes, there’s good reason to think the back pain was the same issue. That’s fuel for another post, but I discussed it here: “Linoleic Acid and Pain”.
Seed Oils and Low-Carb
I’ve often said that I think a good amount of the beneficial effect of a low-carb diet is due to the restriction of seed oils that comes with reducing carbohydrates in ultra-processed foods.
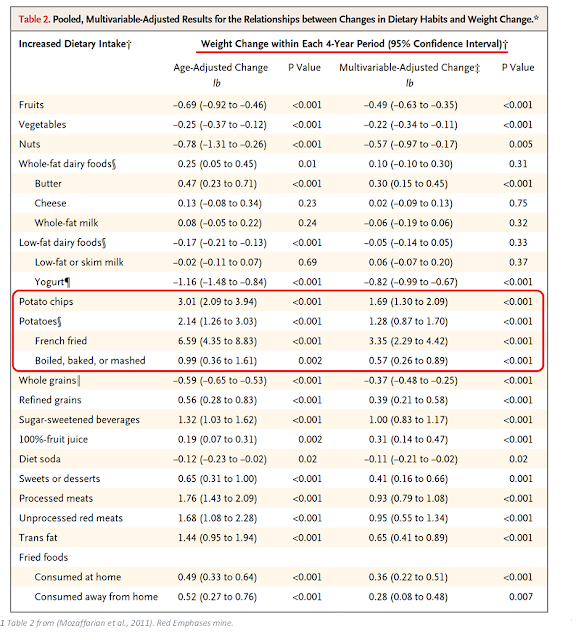
For instance, potatoes fried in seed oils (chips or French-fried) cause obesity, potatoes without seed oils do not.
Dr. Eades’ experience suggests that his low-carb diet has successfully reduced his seed oil intake, and with it his intake of plant-based Ω-3 fats. Soybean and Canola oils are the most common seed oils in the American diet, and have substantial amounts of plant-based Ω-3 fats. For most Americans I suspect those two oils are their primary source of Ω-3 fats. The girl in (Holman, 1982) had her severe Ω-3 deficiency cured with soybean oil.
However, plant-based Ω-3 fats aren’t a substitute for the animal-based variety (Wien, 2010). As in that RCT, eating plant-based Ω-3 fats could have left Dr. Eades with a deficiency, since they do not allow the body to make all the Ω-3 fats it needs. The vegetarians in (Wien 2010) were not able to make DHA from plant-based Ω-3.
How To Get Ω-3
So Dr. Eades, who can eat whatever he would like (I presume), wound up with a deficiency by eating a low-carb, somewhat-processed diet.
“Until I became sensitized to the whole ultra-processed foods idea, I’ve got to admit that I simply looked at the carb content on food labels. I simply read what was in whatever food I was considering in terms of actual food content and completely ignored all the chemicals, gums, preservatives, etc at the bottom of the list of ingredients.”
I presume (I’m doing a lot of that) that means he was eating industrial beef, chicken, and pork, and evidently not enough fish. As Prof. Hulbert notes, that’s a diet that’s deficient in Ω-3.
I have long maintained that fish should not be necessary for a healthy diet. Most of the people in Africa, where we evolved) do not have access to seafood, due to the geography of the continent.
The same is true for every other landmass. If you’re a paleolithic hunter-gatherer, you never popped down to the fish store to buy some for dinner, and it was usually too far a walk to go fishing.
So clearly we had some other way to get it, and that must have been from eating game that fed on leaves and had ample Ω-3 fats, enough to allow us to evolve our large brains.
“The Fat from Frozen Mammals Reveals Sources of Essential Fatty Acids Suitable for Palaeolithic and Neolithic Humans.” (Guil-Guerrero, 2014)
Is Grass-fed Sufficient?
Dr. Eades read Omega Balance recently, and reviewed it in Arrow #202.
He notes a problem with getting enough Ω-3 from modern industrially-raised animals. Is the USDA perpetrating a grass-fed fraud?
“The U.S. Department of Agriculture’s standard for a ‘grassfed’ beef animal is that it be 50% grass-fed.”
WHAT!?!
DRAT. This is very upsetting. But luckily it’s not quite accurate.
The source for this claim is a South Dakota State University Extension website (Bauman, 2021), from which comes the quote above, that ‘grassfed’ means only 50%.
“Information provided in this grassfed beef article series is primarily derived from an April 2017 independent report titled ‘Back To Grass: The Market Potential for U.S. Grassfed Beef’” (Bauman, 2021)
And if one quickly skims that document (Cheung, 2017) one might be left with that impression.
“However, the USDA’s allowance of partial grassfed claims (e.g., “50% grassfed”) and the absence of a requirement for on-farm inspection for grassfed claims mean that not all beef sold with a grassfed label necessarily follows these production standards.” (Cheung, 2017)
And it does have a rather annoying disclosure:
“A striking development in recent years has been the emergence of “grass feedlots,” where cattle are fed grass (often in the form of grass pellets) in confinement. Without mandatory inspection, there is concern that grain byproducts could also be used in these production methods to produce beef labeled as grassfed.” (Cheung, 2017)
But nowhere in this document do they claim that all grass-fed beef is fed 50% grain, or that that is allowed by the USDA.
It’s true that the USDA does allow beef to be marketed as 50% grass-fed:
“When animals have less than 100-percent access to grass or forage the partial “grass fed” claim must accurately reflect the circumstances of raising, e.g., ‘Made from cows fed 85% grass and 15% corn.’” (FSIS, 2019)
And:
“The claim ‘Grass Finished’ is not the same as ‘Grass Fed’ because animals that are ‘grass finished’ can be fed grain, in which case the claim ‘Grain Fed, Grass Finished’ would be truthful and not misleading.” (FSIS, 2019)
However, grass-fed means 100% grass.
“‘Grass Fed‘ or ‘100% Grass Fed‘ claims may only be applied to meat and meat product labels derived from cattle that were only (100%) fed grass (forage) after being weaned from their mother’s milk. The diet must be derived solely from forage, and animals cannot be fed grain or grain by-products and must have continuous access to pasture during the growing season until slaughter. This means 100% grass-fed animals are never confined to a feedlot.” (FSIS, 2019)
It appears that what (Cheung, 2017) claims about grass-fed feedlots is belied by this guideline (no feedlot), but they can be fed hay, grass pellets, and the like, which is reasonable.
What’s more concerning is that the vast majority of grass-fed beef is raised abroad.
“One of the major challenges facing U.S. producers is cheap imports of grassfed beef. These imports account for an estimated 75-80% of total U.S. grassfed beef sales by value. American consumers are often not aware that they are buying imported beef: As long as the imported beef passes through a USDA-inspected plant (which, for food safety reasons, is a requirement for all imported beef), it can be labeled as a ‘Product of the USA.’” (Cheung, 2017)
That’s ridiculous. But from a health perspective, I don’t think it’s a problem. Good beef should be good beef regardless of it’s origin.
Now I don’t know at what point the Ω-3 fats in cattle start to fall as the result of a pellet diet in a grass-fed feedlot. But I’m willing to bet that the Ω-3 fats in grass are one of the first things to go as the grass is dried and aged.
It’s not quite as bad as Dr. Eades’ summation:
“The long and short of it is that you don’t really know what you’re getting when you purchase grass-fed beef.”
I think it’s safe to assume that as grass-fed beef production is industrialized, the Ω-3 content will decline, and there’s no way of knowing exactly what you buy. Fraud in the U.S. food system is widespread, and I think it’s unlikely, given the disparity in price between grass-fed and grain-finished beef, that the beef market is immune.
This makes me think that unless you are able to eat 100% grass-fed beef and dairy and pastured meats it will not be sufficient to give you the Ω-3 you need. And it may not be sufficient even then. The American food system is so corrupted that there is no safe place to go, except for eating fish.
(We’ll get into fish fraud some other time, at least it’s still fish.)
In Arrow #203, Dr. Eades shows a chart from Adele Hite (RIP) that has been used by Peter Ballerstedt in his presentations:
“As you can see, if it is O-6 fats you want to avoid, you could eat 42 (3ounce servings) of grain-fed beef before you would consume as much O-6 as you would get in one tablespoon of soybean oil. And you would have to drink 4 tablespoons of soybean oil to take in the same amount of O-6 fat you would get in 3 ounces of walnuts.
“You shouldn’t agonize over whether to eat grass-fed vs grain-fed beef, since the difference in O-3 fat vs O-6 fat is minuscule. Especially if you’re going to have a salad as a side with some sort of commercially-prepared dressing. You will probably get 30 times more O-6 in the dressing than in the meat.
“You can also see from the slide above that fish are a real bargain when looking to up your O-3 fats without getting a lot of O-6 fats at the same time.
“In the first three fish listed, you would get about the same amount of O-6 fat in the fish as you would in the same size serving of grain-fed beef. But you would be getting a lot more O-3 fat along with it.
“Always consider this second slide when you’re contemplating omega fats. It will tell you vastly more than the O-6/O-3 ratio.”
I re-made this chart to include the Ω Balance, and to sort the data by the amount of Ω-6 in each item, and to normalize soybean oil so it’s also 3 oz, not a tablespoon.
These changes make Dr. Eades’ point about fish vs. beef very obvious. Soybean oil appears as the massive source of Ω-6 fats it is, where in the previous version nuts appeared worst.
It also makes the comparison between farmed salmon and beef, chicken, and pork very easy. Farmed salmon compares quite favorably to a grain-fed ribeye from an Ω-6 perspective, but has 21x the Ω-3.
It also exposes a problem with the Ω Balance, or Ω-6/-3 ratio.
A ribeye and tofu have almost the same Ω balance (13% vs. 12%), but tofu has 4.8x the Ω-6. While tofu also has 4.6x the Ω-3, it’s all plant-based, while the beef has animal-based fats.
Remember, you need the animal-based Ω-3 fats. The plant-based fats in the tofu must be converted, and that conversion is done poorly.
The actual, bioavailable Ω-3 of tofu is a tiny fraction of the 0.46 g/serving shown here. (And that’s not even accounting for the difference in the bioavailability of the protein, or the many other nutritional differences that make beef superior to tofu.)
So while in theory I think this is wrong, “You shouldn’t agonize over whether to eat grass-fed vs grain-fed beef, since the difference in O-3 fat vs O-6 fat is minuscule”, since in theory you should be able to get enough Ω-3 from beef and other ruminants like lamb; in practice here in the United States, I now think this is correct. You will have to get some source of additional animal-based Ω-3 fats, and that’s likely going to be from fish, wild (preferably) or farmed.
It also makes me think that an adjustment to Ω Balance might be in order, to account for the bioavailability.
My Own Rash
Luckily, it’s not on my behind. Instead it’s on the sides of my nostrils and on my forehead, and sometimes on my forefingers.
The one on my nose has been a problem for years, and I’ve tried various lotions for it, including some anti-fungals (a suggestion from a physician many years ago). They do make it better short-term, but are not a cure.
Since reading Omega Balance, I’ve been making more of an effort to include regular fish in my diet, and sure enough, the rash is in a waning stage. It’s not as clear a case as Dr. Eades’, but it’s interesting.
Dermatitis Research
It’s mixed, let’s put it that way. Acute deficiency is covered in Holman’s research above, but the first attempt to induce EFA-deficiency dermatitis in a human failed. However, there are some other epidemiological investigations.
“Based on these results, we consider it plausible that FADS genes and the related PUFA availability may modulate eczema risk.” (Koletzko, 2019)
The FADS gene is involved in converting plant-based Ω-3 to the animal-based ones. Unfortunately, there are many confounding variables here, including baseline consumption of both types of PUFA.
Other research finds a more-consistent, inverse relationship between animal-based Ω-3 levels and dermatitis:
“In this report the severity of eczema and number of allergic symptoms up to two years of age in the infants are related to maternal ω-3 supplementation and maternal and infant DHA, EPA and AA/EPA ratios in plasma phospholipids.” (Furuhjelm, 2011)
So while there are many factors that can drive dermatitis, it’s pretty apparent that insufficient animal-based Ω-3 fat consumption is one of them.
Conclusion
While I am a big fan of low-carb diets, and consider them to be plan A for optimal human nutrition:
I think Dr. Eades’ experience (and mine) shows that it is not sufficient in the context of a industrial American diet. One must take into consideration nutrient availability, including Vitamin F, the essential fats.
A reduced consumption of Ω-6 fats does promote increased Ω-3 status (Taha, 2014). However, in the United States and, likely, other industrial nations, that is not sufficient. Our food supply is too bastardized by the inclusion of mass quantities of Ω-6 fats. Some additional animal-based Ω-3 fats must (it seems) be consumed, and this is most easily done with fish.
Unfortunately we don’t know what is the optimal amount of Ω-3 fats. Until we do, there’s no harm in consuming too much, but this does not mean you must eat nothing but fish.
I will continue to prefer grass-fed beef and dairy, for the better Ω Balance it offers, but my rash suggests that has not been sufficient for me.
I’m reluctant to advise on exact portions, but I now consume fish several times a week, and my favorite sources are canned (in water!) sardines, tuna, and herring (kippers); sushi; and baked or occasionally fried salmon, cod, and haddock. Shellfish are also an excellent, highly-nutritious source of vitamins and minerals, if they are available in your area. I prefer wild-caught, but virtually all salmon in sushi is farmed, and I don’t avoid it.
Fish oil is a distant second as a supplementary source, in my opinion.
That should be enough for one post. Thanks to Dr. Eades for all the material!
References
Bauman, P., & Williams, A. (2021, June 28). Grass-Fed Beef: Understanding Terminology in Conventionally Raised Beef and Grass-Fed Beef [Informational]. South Dakota State University Extension. https://extension.sdstate.edu/grass-fed-beef-understanding-terminology-conventionally-raised-beef-and-grass-fed-beef
Cheung, R., McMahon, P., Norell, E., Kissel, R., & Benz, D. (2017, April). Back to Grass: The Market Potential for U.S. Grassfed Beef. Bonterra Partners & SLM Partners. https://www.stonebarnscenter.org/wp-content/uploads/2017/10/Grassfed_Full_v2.pdf
Food Safety and Inspection Service. (2019, December). Food Safety and Inspection Service Labeling Guideline on Documentation Needed to Substantiate Animal Raising Claims for Label Submissions. U.S. Department of Agriculture. https://www.fsis.usda.gov/sites/default/files/media_file/2021-02/RaisingClaims.pdf
Furuhjelm, C., Warstedt, K., Fagerås, M., Fälth-Magnusson, K., Larsson, J., Fredriksson, M., & Duchén, K. (2011). Allergic Disease in Infants up to 2 Years of Age in Relation to Plasma Omega-3 Fatty Acids and Maternal Fish Oil Supplementation in Pregnancy and Lactation. Pediatric Allergy and Immunology, 22(5), 505–514. https://doi.org/10.1111/j.1399-3038.2010.01096.x
Guil-Guerrero, J. L., Tikhonov, A., Rodríguez-García, I., Protopopov, A., Grigoriev, S., & Ramos-Bueno, R. P. (2014). The Fat from Frozen Mammals Reveals Sources of Essential Fatty Acids Suitable for Palaeolithic and Neolithic Humans. PLOS ONE, 9(1), e84480. https://doi.org/10.1371/journal.pone.0084480
Holman, R. T. (1971). Essential Fatty Acid Deficiency. Progress in the Chemistry of Fats and Other Lipids, 9, 275–348. https://doi.org/10.1016/0079-6832(71)90030-9
Holman, R. T., Johnson, S. B., & Hatch, T. F. (1982). A Case of Human Linolenic Acid Deficiency Involving Neurological Abnormalities. The American Journal of Clinical Nutrition, 35(3), 617–623. https://doi.org/10.1093/ajcn/35.3.617
Holman, R. T. (1998). The Slow Discovery of the Importance of ω3 Essential Fatty Acids in Human Health. The Journal of Nutrition, 128(2), 427S-433S. https://doi.org/10.1093/jn/128.2.427S
Hulbert, A. J. (2023). Omega Balance: Nutritional Power for a Happier, Healthier Life. Johns Hopkins University Press. https://amzn.to/3uC2igY
Koletzko, B., Reischl, E., Tanjung, C., Gonzalez-Casanova, I., Ramakrishnan, U., Meldrum, S., Simmer, K., Heinrich, J., & Demmelmair, H. (2019). FADS1 and FADS2 Polymorphisms Modulate Fatty Acid Metabolism and Dietary Impact on Health. Annual Review of Nutrition, 39(1), 21–44. https://doi.org/10.1146/annurev-nutr-082018-124250
Taha, A. Y., Cheon, Y., Faurot, K. F., MacIntosh, B., Majchrzak-Hong, S. F., Mann, J. D., Hibbeln, J. R., Ringel, A., & Ramsden, C. E. (2014). Dietary Omega-6 Fatty Acid Lowering Increases Bioavailability of Omega-3 Polyunsaturated Fatty Acids in Human Plasma Lipid Pools. Prostaglandins, Leukotrienes, and Essential Fatty Acids, 90(5), 151–157. https://doi.org/10.1016/j.plefa.2014.02.003
Wien, M., Rajaram, S., Oda, K., & Sabaté, J. (2010). Decreasing the Linoleic Acid to α-Linolenic Acid Diet Ratio Increases Eicosapentaenoic Acid in Erythrocytes in Adults. Lipids, 45(8), 683–692. https://doi.org/10.1007/s11745-010-3430-3











From personal experience, I vaguely disagree: even eating wild salmon daily, I got sunburn back (after it went away on a low-PUFA diet), felt vaguely more inflamed/uncomfortable.. I also seem to remember farmed salmon being about 1:1 on o3 and o6, though I don't recall the study now. It had pictures of salmon fillets, maybe even on your blog?
In addition, irrespective of their omega balance, farmed (aka nearly all) Atlantic salmon are raised in disgusting conditions, much worse than pretty much any other mass meat production method.
I have also read that "wild caught" salmon is often a scam, that they released farmed salmon and then re catch them to mark as "wild caught."
Intriguingly, I got dry skin after going on a low-fat (<1%) rice based diet for a month recently. Cleared up as soon as I went back on the cream diet.
edit: found the study, yep 1:1 o3:o6 in farmed norwegian salmon
https://onlinelibrary.wiley.com/doi/10.1002/fsn3.2911
I come from an area the raises beef. If beef is pure grass fed, you can see the difference, the fat tends to be more yellow and is a different texture.
It takes twice as long to raise beef on grass vs the usual feed - thus real grass fed is about twice as expensive to raise - and it sells for about 2x the price.
Would people lie to get twice the money out of the sale? Sadly yes. And it is harder to be virtuous when living in the third world where a lot of our beef comes from.